Skin Biopsy
Reviewed by: HU Medical Review Board | Last reviewed: May 2017. | Last updated: May 2019
A skin biopsy is a procedure in which your doctor removes a sample of skin tissue. The sample is sent to a laboratory. A pathologist will examine it under a microscope. By looking at the cells in the sample, the pathologist can diagnose or rule out skin cancer. If your doctor removed the entire lesion, then the biopsy may also have cured the cancer.
Skin biopsy is a simple procedure that is usually done in your doctor’s office. Dermatologists and some primary care providers do skin biopsies. There are different skin biopsy procedures. The type of biopsy is chosen based on the lesion size and location, as well as the suspected type of skin cancer.1,2 Suspected melanomas are treated differently than suspected non-melanomas. Your doctor decides how likely melanoma is based on lesion features and your personal risk factors.
What are the types of skin biopsy procedures?
Skin biopsy procedures can be grouped by how much of the lesion is removed.1 If you have an excisional biopsy, the entire lesion is removed. Examples of excisional biopsy procedures include elliptical excision, deep scoop shave, and punch biopsy for small lesions. If you have an incisional biopsy, only part of the lesion is removed. Examples of incisional biopsy procedures are superficial shave or partial punch biopsy.
Superficial shave. A superficial shave biopsy is quick and simple to perform. Your doctor will use a scalpel, razor blade, or scissors to remove a thin disk of tissue.1 Superficial shave biopsy is used only for lesions located entirely in the epidermis, the top layer of skin. For example, it might be used for suspected basal cell carcinoma, squamous cell carcinoma, or actinic keratosis. This procedure would not be used for suspicious pigmented (dark) lesions.1 Follow your doctor’s instructions for wound care after a superficial shave biopsy. Usually you will be instructed to keep the site covered for 1 week and use an ointment to keep it moist.1
Deep scoop shave. A deep scoop shave is considered an excisional biopsy procedure. Your doctor will use a large, curved blade to remove a thick disk of skin. The incision may go into the dermis or the fat layer under the skin (subcutaneous fat).1 Another name for deep scoop shave biopsy is saucerization.
Deep scoop shave can be used for suspected melanomas. It is particularly useful for melanomas on the upper back, shoulders, chest, upper arms, lower legs, and ears.1 You will not need stitches after a deep scoop biopsy because the wound will close on its own. Compared with elliptical excision, deep scoop shave biopsy leaves a rounder, smaller scar.1
Your doctor will tell you how to care for the wound after a deep scoop biopsy. Just like a superficial shave biopsy, you probably will be told to keep the site covered and use an ointment.2
Punch biopsy. Your doctor will perform a punch biopsy using a special instrument with a circular blade.1 Your doctor will place the instrument over the lesion and rotate it around.2 The instrument is rotated downward until it reaches the fat layer underneath. This technique produces a cylindrical (tube-shaped) tissue sample. This type of biopsy is useful when a sample of the dermis or fat layer is needed.1
Punch biopsy may be incisional or excisional, depending on the size of the lesion.1 This procedure may be used to take a sample from a large lesion, if that lesion is unlikely to be melanoma.1 If the lesion turns out to be cancerous, a second surgery will be scheduled to remove the entire tumor. Punch biopsy can also be used for excisional biopsy of small suspected melanomas. In this case, the whole lesion is removed.
The biopsy site is closed with a few stitches. Your doctor will instruct you on how to care for the site. Typically, you will be asked to keep the site covered and dry for 24 hours.1
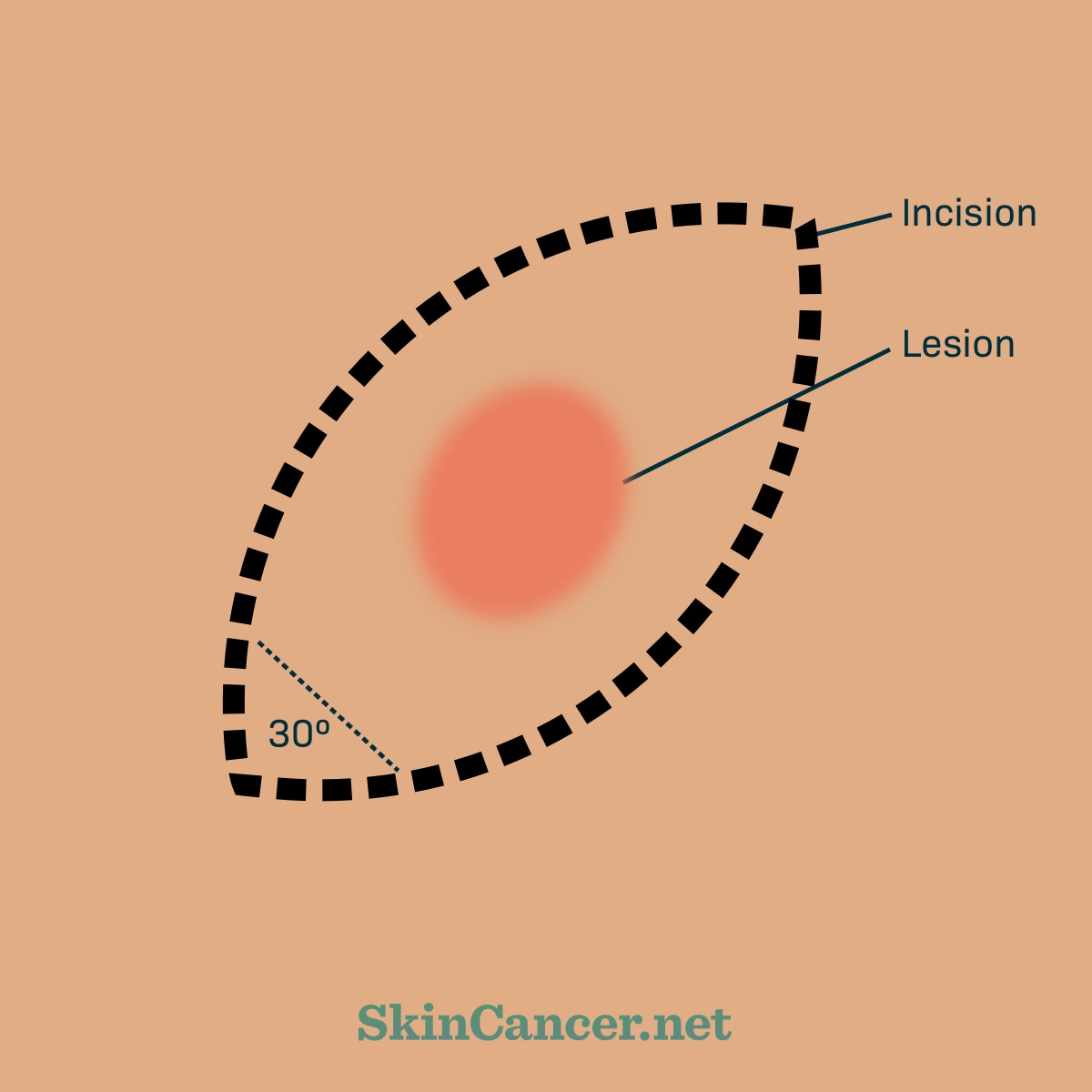
Elliptical excision. To do an elliptical excision, the dermatologist will draw a 1 to 3 mm outline (margin) around the suspected melanoma.2,3 Margins are the healthy skin around the tumor that is cut out. Then your doctor will cut an elliptical (football) shape around it. An elliptical cut removes more skin than a circle would, but results in a better looking scar.4 Another term for elliptical excision is fusiform excision. Your doctor will close the wound with stitches.4 You may need to return to have the stitches removed. Your doctor will tell you how to care for the wound. Typical instructions are to keep the incision clean and dry for 36 hours. Then keep it covered for a few more days.
Figure 1. Elliptical excision
Source: http://img.medscapestatic.com/pi/meds/ckb/80/10280tn.jpg
Doctors consider elliptical excision to be the best way of taking a biopsy from a suspected melanoma.2 Because the sample contains the full lesion, the dermatopathologist can study the tumor edges and thickness.2 With incisional biopsy, there is always a risk that the sample does not actually represent all the cancer cell types. A sample obtained by elliptical excision is sure to have all cancer cell types.
The difference between elliptical excision for biopsy and wide excision for treatment is the width of the margins.1 One reason biopsy margins are narrow is to avoid disturbing the lymph vessels. Preserving normal lymph flow may be important if you need a sentinel node biopsy.3 Narrow margins create a smaller scar. If the lesion is cancerous, you probably will have a second surgery (re-excision) to remove any remaining cancer cells.
What happens during the appointment for skin biopsy?
It is common practice to photograph a lesion before it is biopsied.5 This helps the surgeon find the site later if additional surgery is needed.
Your doctor will clean and numb the area.1 The biopsy procedure will be performed. Your doctor will stop the bleeding using medication, cauterization, stitches, or surgical adhesive. Your doctor will apply ointment and a bandage. The sample will be processed and sent to a laboratory.
How is the sample studied?
A pathologist or dermatopathologist will study the sample under a microscope. The pathologist will identify which cells have grown abnormally. Features of the cancer seen under the microscope will be described in the pathology report.
It may be necessary to run tests on the sample to make a diagnosis. These tests may include:
- Immunohistochemistry (IHC): A lab test that checks cells for antigens (markers of melanoma)
- Fluorescence in situ hybridization (FISH): A laboratory technique for seeing the genes or chromosomes in a sample of cells. Chromosomal abnormalities are a sign of cancer. Certain abnormalities are typical of melanoma.
- Molecular testing: For advanced melanoma, a variety of tests may be used to evaluate changes in the DNA copy number or specific DNA mutations.
How do I find out the biopsy results?
The pathologist will summarize the findings in a pathology report.6 The report will include a diagnosis and a description of the cancer. This description will include information about the tumor thickness and margins, how quickly the cancer cells are dividing (mitotic rate), and whether the top layer of cells has broken down (ulceration). The pathology report may also include factors such as:
- Invasion of the tumor into a nerve, blood vessel, or lymph vessel
- Presence of tiny tumors near the main tumor (microsatellitosis)
- Presence of immune cells in the tumor
Information from the pathology report is used to stage the cancer and determine the course of treatment. Your doctor will go over the pathology report with you.
What are the risks or harms of skin biopsy?
Skin biopsy leaves a scar.7 Before the procedure, you may want to discuss the expected appearance of the scar with your doctor. Other risks of a skin biopsy are bleeding or infection. Tell your doctor if you have a history of bleeding problems.
A concern about incisional biopsy is that it could lead to difficulty staging melanoma later. If melanoma is partially removed, it may not be possible later on to figure out how deep the tumor was at its thickest point. The “T” category in the TNM staging system is based on tumor thickness. For this reason, excisional biopsy is preferred for suspected melanoma.1
What questions should I ask my doctor about skin biopsy?
It is a good idea to ask questions before any procedure, even simple office-based procedures such as skin biopsy. Consider asking questions such as:
- What information will this biopsy provide?
- What procedure will you use? Are you planning to remove part or all of the suspicious lesion? What is your reason for that?
- What are the alternatives to skin biopsy?
- How will the scar look when the incision has healed?
- How many of these procedures have you done?
- How should I take care of the incision?
- How long does it normally take for this type of biopsy to heal?
- What should I do if the incision starts to bleed?
- What are signs of infection? How will you treat an infection?
- Will I be in pain after the procedure?
- What activities should I avoid after the procedure? For how long?
- Can I bathe or shower?
- When and how will I get the results of the biopsy?
- If the biopsy shows that I have cancer, what additional surgery or tests will I need?